Trichomonas is Common
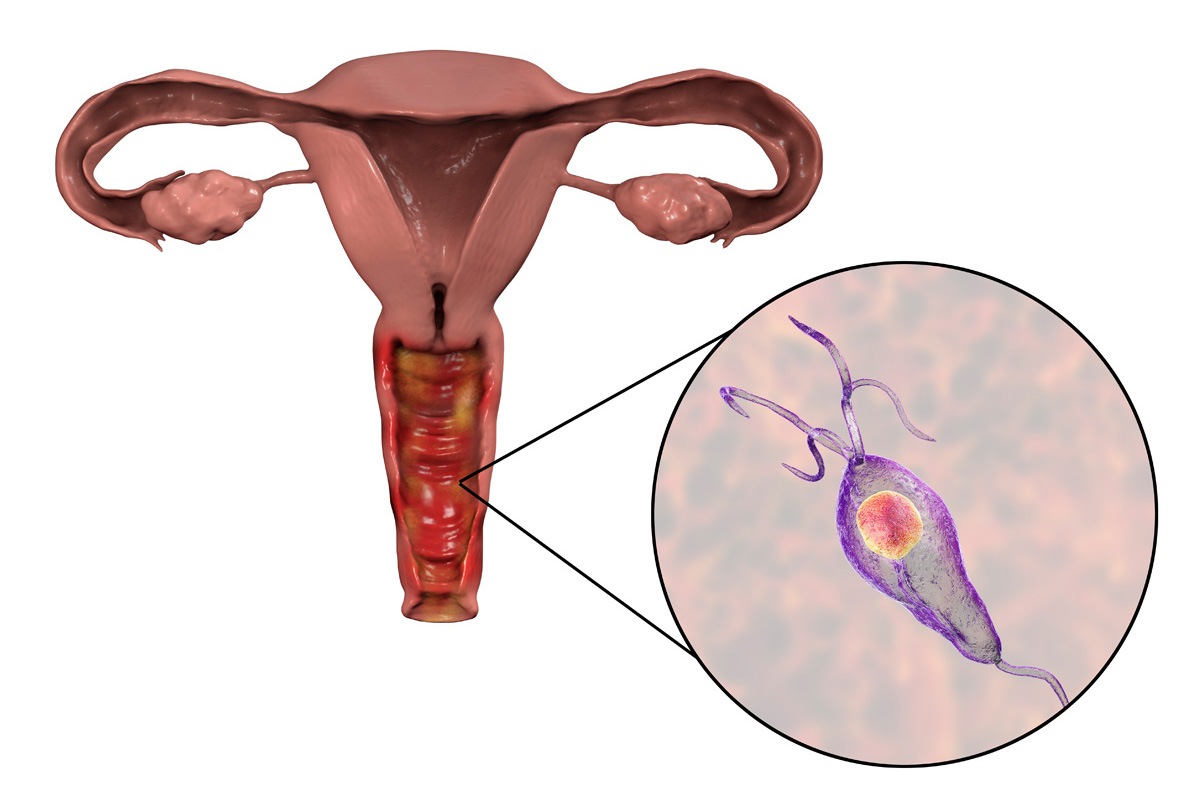
Trichomoniasis, commonly known as “trich,” is one of the most common sexually transmitted infections (STIs). It is caused by a one-celled parasite, Trichomonas vaginalis. Men and women are affected by this infection, but it occurs more often in women.
Anyone engaging in sexual activities is at risk of infection with T. vaginalis, but some groups have a greater likelihood. Older women and African American women are at more risk.1
In the US, trichomoniasis is one of the most curable, non-viral STIs.2,3 Unfortunately, this infection is not well researched, primarily because trichomoniasis is not identified as a reportable condition by the Centers for Disease Control and Prevention (CDC).
In 2018, there were an estimated 6.9 million cases of diagnosed and undiagnosed T. vaginalis infection in the US population.
Based on this data, the T. vaginalis infection is the third most common STI in the US population (the first two are human papilloma virus and herpes simplex virus-2, a compelling reason to promote more research and testing for trichomoniasis.(3,4)
Trichomonas Symptoms
Most people with trichomonas (70%)1,2 won’t experience any symptoms related to this infection. For those who experience symptoms, these begin days or weeks post infection.1 It is advisable to recommend regular testing because untreated infection increases the risk of getting or spreading trichomonas and other STIs, for example, HIV.1
In many cases, asymptomatic women can become carriers for the infection for more than three months.5 Without treatment, the infection in women may go unnoticed for years.2 Most men (more than 75% of the cases) are believed to have asymptomatic as well as transient infections with resolution of the infection within ten days.5

Women with trichomoniasis can experience the following:1
- Vaginal discharge with foul odor and yellow or greenish color
- Pain when urinating or during sexual intercourse
- Genital itching, soreness, redness, or burning
- Bleeding after intercourse
- Urinary urgency
Symptomatic men can experience the following:
- Pain or irritation when urinating
- Itching or irritation inside the penis
- A thin white discharge from the penis
Trichomonas Transmission
Like all STDs and STIs, trichomonas is transmitted through sexual intercourse. An individual can get infected by having a sexual encounter with someone who has trichomoniasis. Typically, the infection gets transmitted through vaginal sex.1
It is also possible for a woman to get infected during intercourse with another woman through vaginal contact. Women get the infection primarily in their vulva, vagina, cervix, and urethra. Men get the infection in their urethra and, sometimes, prostate.1
An individual doesn’t have to experience any symptoms to transmit the infection.1
Long-Term Risks and Complications of Trichomonas
Because trichomonas is often an asymptomatic infection, it is harder to diagnose and treat. Unfortunately, this can lead to long term harm because infected people can experience some significant complications from trichomoniasis.
One of these complications is an increased risk of getting and/or spreading other STIs. There is a two to three times higher risk of contracting HIV when infected with trichomonas.6
Women who plan to get pregnant or already are pregnant must be aware of complications related to trichomoniasis. This infection can increase the risk of premature birth by up to 30%.6 This, of course, may lead to many more difficulties for the infant (for example, low birth weight).7 There is also a slight risk of the infant becoming infected during a vaginal delivery.1 Women with trichomonas infection are at a greater risk of cervical neoplasia, infertility, and pelvic inflammatory disease.8
Trichomonas Diagnosis
There are a few ways to detect the infection. One of the most common is for an individual to provide a urine or genital sample. Wet mount can detect the parasite.1 This test is simple and inexpensive with rapid results. However, it has low sensitivity and is inaccurate in men.9
T. vaginalis can be cultured. This test can be used to diagnose men and women. However, it also requires trained personnel, special equipment, and results can take up to seven days.9
Very effective tests for the presence of the T. vaginalis parasite are Nucleic Acid Amplification Tests (NAATs). This method is one of the best ways to diagnose people, primarily because of the heightened sensitivity of these tests.9
NAATs can be conducted in clinical and non-clinical settings. This test uses vaginal or endocervical swabs, urine samples, or urethral swabs, and it is designed to detect the presence of the T. vaginalis parasite DNA or RNA sequence.10 This method can be used to diagnose women and men. The downsides to NAATs are they can be expensive, require laboratory equipment, and results can take several days.9
Antigen Tests can be performed only on symptomatic women (it is not approved for men and asymptomatic women). This test offers same-day results, so it might be a good alternative to other methods that take more time.9
Trichomonas Treatment
To clear the infection, an individual needs antibiotic therapy. The most common medication prescribed for trichomonas is metronidazole or tinidazole. All the prescribed antibiotics must be taken for effective treatment of the infection.1

It is also vital that all sexual partners get treatment. There is a high risk of reinfection with trichomonas when treatment is not completed. It is reported that about 20% of people get the infection again after completing treatment.1
Tinidazole is not recommended for pregnant women.11
It is essential for women to have follow-up testing three months after ending treatment. Men don’t have this requirement. It is also recommended to limit all sexual activity for the duration of the treatment (usually, it’s seven days).11
Trichomonas Infection Prevention
As for the prevention of trichomonas, the same rules apply as with practicing safe sexual activity. People can abstain from engaging in risky sexual behaviors, use condoms as protection from STDs and STIs, and choose to have intercourse with a limited number of uninfected partners.11
It is also advised that people get regular testing and only engage in sexual activities with people who also undergo regular testing. Women with HIV are at greater risk, so they are recommended to test at least once a year. Regular testing is also recommended for individuals with high-risk professions, for example, sex workers.5
Final Thoughts
Trichomonas is a fully treatable and manageable condition, but it comes with potential long-term complications. Regular tests and increasing awareness of this condition are entirely justified.
Since trichomonas infection is one of the most common STIs in the US, and fact that the CDC does not pay it enough attention, promoting testing and enabling people to get tested using more accessible tools is warranted.
The Visby Medical Sexual Health Click Test is easy to use and provides results in under under 30 minutes. Thanks to that, you can provide your patient with results during the same appointment and go over the next steps. Read more about our test and improve your quality of care.
References
- Trichomoniasis (Trich), WebMD website: https://www.webmd.com/sexual-conditions/guide/trichomoniasis, Accessed May 12, 2022.
- Trichomoniasis – CDC fact sheet. Centers for Disease Control and Prevention website. https://www.cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm. Reviewed January 19, 2021, Accessed May 12, 2022.
- Kreisel KM, Spicknall IH, Gargano JW, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex Transm Dis. 2021;48:208-214.
- Sexually transmitted infections prevalence, incidence, and cost estimates in the United States. Centers for Disease Control and Prevention website. https://www.cdc.gov/std/statistics/prevalence-2020-at-a-glance.htm. Reviewed January 25, 2021, Accessed May 12, 2022.
- Sobel JD, Mitchell C. UpToDate: Trichomoniasis. Wolters Kluwer website. https://www.wolterskluwer.com/en/solutions/uptodate. Updated April 20, 2021. Accessed May 12, 2022.
- Van Gerwen OT, Muzny CA. Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000 Research. 2019;8:1-9.
- Blundell O, AWG Languedoc-RoussillonF. The impact of sexually transmitted infections (STIs) on women’s health. FAWCO website. https://www.fawco.org/global-issues/health/health-articles/4051-the-impact-of-sexually-transmitted-infections-stis-on-women-s-health. February 25, 2019, Accessed May 12, 2022.
- Patel EU, Gaydos CA, Packman ZR, Quinn TC, Tobian AA. Prevalence and correlates of Trichomonas vaginalis infection among men and women in the United States. Clin Infect Dis. 2018;67:211-217.
- Hobbs MM, Seña AC. Modern diagnosis of Trichomonas vaginalis infection. Sex Transm Infect. 2013;89:434-438.
- Garcia MR, Wray AA. Sexually transmitted infections. NCBI website. https://www.ncbi.nlm.nih.gov/books/NBK560808/. Updated July 15, 2021, Accessed May 12, 2022.
- Spach DH. Vaginitis: trichomoniasis. National STD Curriculum website. https://www.std.uw.edu/go/syndrome-based/vaginal-discharge/core-concept/all#trichomoniasis.Updated October 12th, 2021, Accessed May 12, 2022.